Introduction: Heavy Menstrual Bleeding (HMB) is one of the most common indications for ambulatory gynecological visits amongst reproductive aged women. It can have significant physical, social, emotional, and economic impact. Two thirds of women who report HMB develop anemia. While the outpatient setting may represent the optimal setting for management of this condition, it is known that many patients are treated in the emergency room or inpatient setting. We sought to evaluate Emergency Department (ED) utilization and the associated health care charges of patients who present to the ED with HMB. We hypothesized that marginalized groups are more likely to use the ED for HMB and are more likely to be admitted for this condition.
Methods: The Nationwide Emergency Department Sample (NEDS) Database of the Health Cost and Utilization Project (HCUP, Rockville, MD) was queried for all visits with primary ICD-10 diagnosis codes of N92.0 (Excessive and Frequent Menstruation with Regular Cycle) or N92.4 (Excessive bleeding in the premenopausal period) among females 21-50 years of age. Variables assessed included age, hospital type, medical insurance, household income quartile, visit charges, disposition, and race. Race data were only available for 2019 and 2020. Z-test and Chi-square analyses were performed to compare counts and proportions across groups and years. All analyses were performed using SAS 9.4 (Cary, NC).
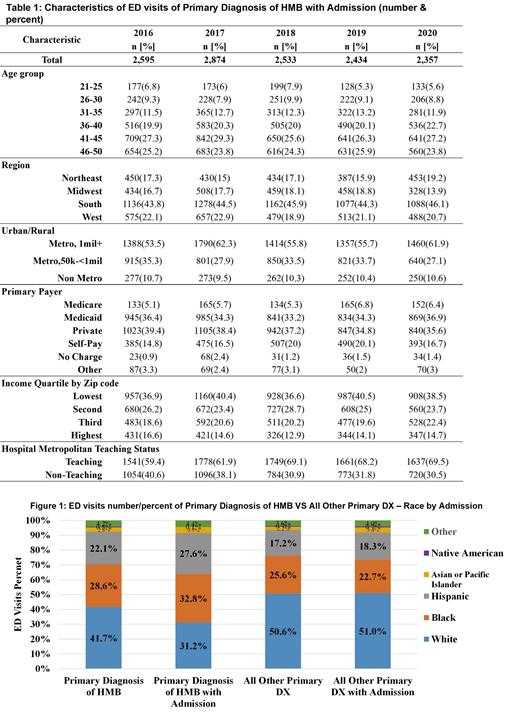
Results: Between 2016 and 2020, 195,499 emergency room visits with a primary diagnosis of HMB were identified out of 164,441,890 total ED visits (0.12% of visits). The patient mean (SD) age was 33.7 (0.1) years. Total ED visits per year for HMB declined from 42,462 in 2016 to 33,718 in 2020. Self-pay represents a disproportionately high share of admissions. Approximately 6% of patients who presented to the ED with HMB were admitted which was stable from 2016-2020. Patients age 21-25 years represented the highest proportion of ED visits for HMB with 21.5% versus 12.2% among those ages 46-50 years. However, patients age 46-50 years accounted for 24.6% of admissions versus 6.3% of admissions for those aged 21-25 years. Patients 46-50 years had the highest admission rate (13.2%) versus 1.9% for ages 21-25 years. HMB related charges were over $150,000,000 per year, with a median charge per visit of over $3,000. For the two years for which race data were available, White women (WW) represented 41.2% of HMB visits versus 50.6% of all other diagnoses visits; Black women (BW) represented 28.6% of HMB ED visits versus 25.6% of all other diagnoses, and Hispanic women (HW) 22.1% of HMB ED visits versus 17.2% of all other diagnoses. Of the patients that were admitted for HMB, 31% were White versus 51% of all other diagnoses admissions, 33% were Black compared to 23% of all other diagnoses admissions, and 28% were Hispanic versus 18% of all other diagnoses admissions. Admission rates were higher for Black/Hispanic/Asian-Pacific Islanders (7.6%, 8.2%, 9.1%) vs. WW (4.9%). Percentage of ED visits for HMB for BW and HW were 29% and 22% respectively which compared to 25.6% and 17.2% of visits for all other diagnoses.
Conclusion: ED visits with HMB as a primary diagnosis represent a small percent of visits overall and are decreasing. However, Black and Hispanic patients make up a disproportionate percentage of HMB patients. In addition, there is an inverse relationship with respect to age between ED visits and admissions. Younger adults ages 21-25 years make up the highest percentage of ED visits by age, but they are the least likely to be admitted with an admission rate of 1.9% suggesting an opportunity to better leverage an outpatient visit setting for this demographic. This analysis serves as a first step to understand ED utilization for HMB, and suggest potential disparities in ED utilization and/or admissions for HMB by age and race. Given the overall low admission rate, there may be an opportunity to improve outpatient services for HMB in younger women and in Black and Hispanic women.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal